This post shares a video and transcript of my speech at the emergency demonstration in George Square, Glasgow, on 18 April 2024, against the decision from NHS Greater Glasgow and Clyde to ban endocrine treatments for trans people aged under 18. The speech was unplanned and made without notes, so I have made some small corrections in the transcript, plus minor amendments for clarity. I have also added references for some key points. Thank you to @transprotestglasgow for the video.
Readers seeking more detailed evidence and academic critiques may find my previous blog post helpful: What’s wrong with the Cass Review?
Hi, I’m Ruth Pearce.
I’m a Lecturer in Community Development at the University of Glasgow, and I’m a researcher on trans healthcare.
And I was a trans child.
I want to talk about that for a moment. Because I came out to myself circa 2001, when I was 15, when not many people did that. And it was hard for us. And there was trans community, and there was information, but it was very difficult because we felt very, very alone. I was mostly only able to connect with other trans people my age through the internet, through blogs, and they were mostly Americans. The Brits were there; a lot of us connected later as we grew older. But we were so isolated.
A really important thing to remember, in a moment like this where we are seeing a return to the kind of medical policies that were in place when I was a kid: there are so many more of us, and we are so much more powerful than we have ever been.1 Never forget that strength we have together.
One of the things Hilary Cass says in her report is that the meaning of the word “trans” has changed since 2020.2 She says, and there is no evidence for this, that “trans” in 2020 meant something quite rigid and specific, and only now in 2024 it’s become an umbrella term for lots of identities. Tell that to me coming out as a trans teenager in 2001!
So here’s the thing. We’ve always been here, and we are more powerful now, but we are seeing this backlash. That’s been a long time coming and transphobia changes its face over time. One of the things I wanted to do to deal with my loneliness and the experiences I had was that I wanted to become an activist. And when I started doing activism, when I got into meetings with people in government, and with the Equality and Human Rights Commission, they said “there’s no evidence” for the discrimination we faced. So I was like, “fine: let’s see what evidence I can find”.
So I did a PhD in trans healthcare.3 And I found what you often find when you do research; you often find things you don’t expect. So I did find some things I expected to find. About waiting lists and how hard they are. About how hard appointments can be when you’re meeting with sexist and transphobic clinicians who are asking you, as a young person, how you masturbate and who you’re attracted to. But what I didn’t expect was the sheer level of pain from the waiting. And I talk about that in my work. And the anticipation, where we are anticipating all the time. When is it going to happen? When are we going to get to live our lives? And that happens on every level of our lives.
I was also shocked by the level, and detail, and complexity of the ignorance of healthcare practitioners. It ranges: it’s not just that they all hate us, right? It’s that some people are trying to control us, some people want to help but don’t understand how, and some people don’t want to know. There’s different kinds of ignorance.4
So I published my work, and other people have followed. Other people were there before me of course, because “trans” was not new, and trans research wasn’t new either. There is now a lot of published research on what it is like to go through a gender clinic, and what it is like for a young person to go through a gender clinic. There’s people like Cal Horton5 and Natacha Kennedy6 who are writing on this, and Harvey Humphrey7 who works here in Glasgow. There’s a lot of people doing work on this.
We are saying, time and time again, “we need services that meet our needs”. For some people, that is access to puberty blockers, and that is access to hormones. For other people, that is access to counselling, and therapy, and community support. What we call “trans-affirmative” or “gender-affirmative” care is flexibility, meeting a person where they are at, and based on what they want to do with their lives.8 You don’t have to change your body – but you can.
It’s our body, it’s our right: we can do what we want with our own bodies.
This is what is disgusting about the decision by NHS Greater Glasgow and Clyde. They have not addressed the years and years of mistreatment and abuse in their child and adolescent clinic at Sandyford. It is not a great place that we are trying to save. It is a clinic that has repeatedly refused to treat young people, and made people hold on for care. It has helped a handful of people. Dozens of people – only dozens – have accessed treatment in the last few years.9 Now they are proposing to stop doing the very little they are doing to support young trans people.
People who get a referral to a child and adolescent gender clinic are not necessarily seeking access to counselling and therapy, because you can get that elsewhere.10 They are not seeking access to community, because you will find no community at Sandyford. They are most likely seeking access to endocrine treatments: puberty blockers and hormone therapy. And that’s what they are going to stop doing.
Sandyford say they are still accepting new referrals. But what is the point of a gender clinic that does not offer people medical treatment?
NHS Greater Glasgow and Clyde have based their decision on the final report of the Cass Review. Let’s talk a bit about the Cass Review.
I’m an academic researcher. If the Cass Review was submitted by an undergraduate student, the first thing I would say is: “That’s nearly 400 pages long! No-one’s going to have time to mark that”.11 And you’ll notice that all the people in the media, all the Labour politicians, all the Tory politicians, all the people saying we should immediately implement the findings of the report: none of them read nearly 400 pages in one day. Neither did the journalists at the BBC, the Telegraph, the Times, the Daily Mail, the Observer, the Independent. We expect better! And now the Scottish media: it’s all over the Scotsman, the National, the Herald. None of them have bothered to read the report, or think about it critically.
So here’s a bit of information about the Cass Review. The Cass Review was undertaken by a group of people who, from the very start, excluded trans people from oversight of the project. That was in their terms of reference.12 They didn’t want people who had experienced services having a formal part in the report. They excluded healthcare experts. If you were someone who had worked in a gender clinic you were excluded from being part of that.13 You know, I have lots of disagreements with many people who work in gender clinics, but you would have thought they might get a say.
You can see that ignorance, that intentional ignorance, playing out in the final report of the Cass Review. You can see, if you read the Cass report, that they looked at over 100 studies, most of which show that puberty blockers and hormone therapy can help young trans people. And they just ignored them.14 Intentionally. They say that the majority were not “high quality evidence”.15
What else is not high-quality evidence in healthcare? Paracetamol for back pain.16 There is no high quality evidence for that, in the terms of the Cass Review. Anti-psychotics.17 ADHD medication.18 All these medications that are in regular use. You know what else? Puberty blockers for young people with precocious puberty – if they’re cis.19 That is direct discrimination. 20
The thing is, that’s the Cass Review being serious. Let’s think about when it gets weird.
There’s a graph in there, where they show referrals to a gender clinic (the Gender Identity and Development Service in England) rising year on year, with “an exponential rise in 2014”. But they cut the graph off at 2017. But if you look at 2017-2020 the referral rate flattens off. It’s deliberate removal of evidence.21
We know why this is happening. Experts – medical experts, and experts by experience have been cut out of the Cass Review process. If you are trans, that’s you. You are an expert by experience. You know what it’s like. We have been cut out the process!
And the NHS have done that here in Scotland. There was no consultation on the ban that’s come in.
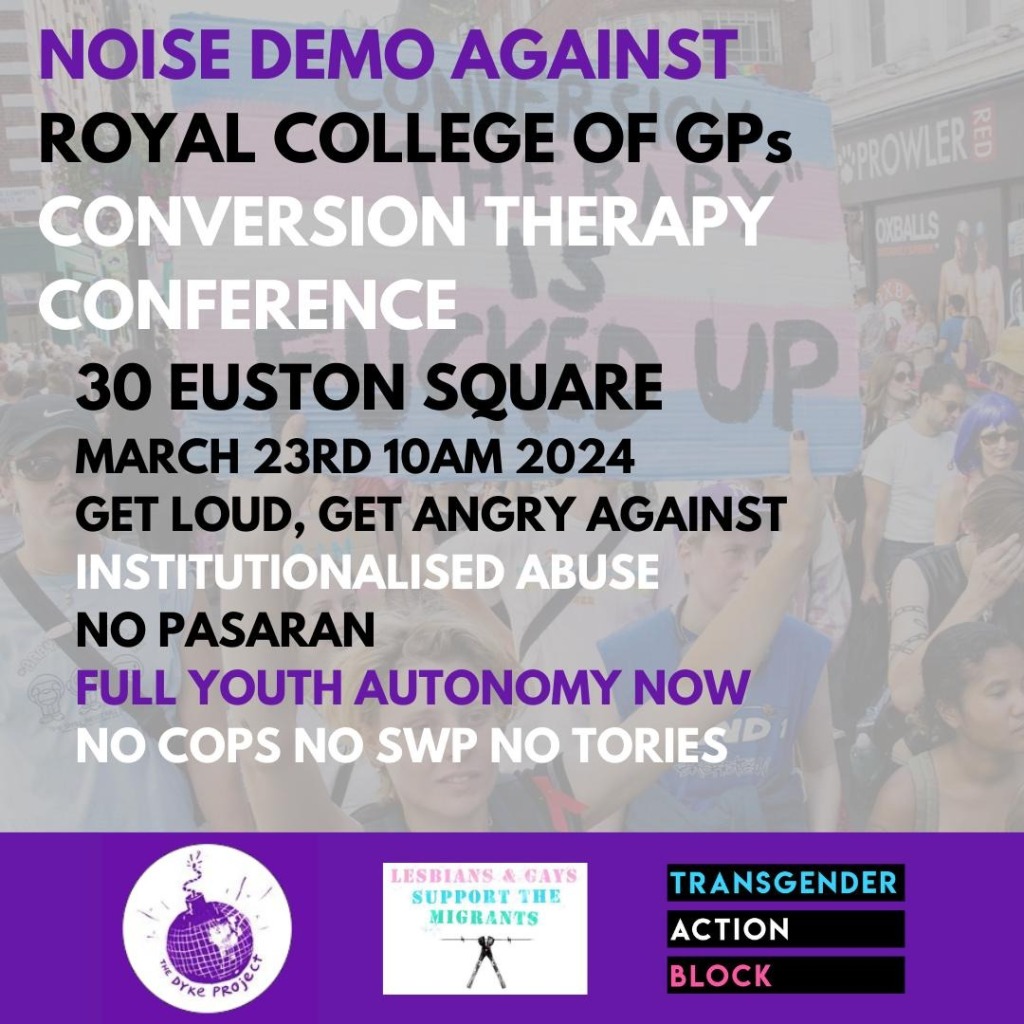
Who did they consult? We know there are people who are proponents of conversion therapy who were on the Cass Review team.22 That is what they are proposing.
They are proposing conversion therapy. Not just for trans kids, because they want to deal with all gender-questioning and non-conforming kids. This is going to be conversion therapy for queer kids. Little boys who want to wear a dress, they might not be trans, but they deserve to have the space to explore. That is not going to be what happens in clinics where people are referred which are being informed by conversion therapists.23
So consequently you have other weird stuff in the Cass Review. They’re dismissing all the evidence about why puberty blockers and hormones can benefit people within particular contexts, but they’re relying on other evidence for their recommendations. Let me give you one citation. “Thoughts on Things and Stuff, 2023”. That is a citation from the Cass Review: Thoughts on Things and Stuff.24
What is “Thoughts on Things and Stuff”? It’s a right-wing Youtube channel run by anti-trans bigots,25 featuring contributors such as “Gays Against Groomers”.26 This is the level of evidence that is informing NHS Greater Glasgow and Clyde.
And I’ll tell you what else is in the Cass report. They say that little girls are likely biologically inclined to play with dolls. It’s right in there, in the Cass report.27 And little boys are probably biologically inclined to play with trucks. Why is this? It’s not just an anti-trans agenda. It’s an anti-feminist agenda. Its an anti-woman agenda.
Why is this happening? It’s happening because trans people are an easy target.
If you want to stop young people accessing contraception as teenagers, you remove trans people’s right to consent to care as young people. If you want to prevent young people – teenage girls – from having abortions, and you’re failing time and time again in the courts, you instead target puberty blockers, because that way you can set a precedent for preventing people from being able to make decisions as young people. You are undermining the idea that young people might have the capacity to consent to care and make an informed decision about their own bodies.28
So I will end on this. I’m a woman, I’m a trans person, and I think it’s really important we think about allies. I had the parent of a trans child contact me and say, “thank you for being an ally”. I want to think her for being an ally. The thing about allies is, we talk a lot about an “ally” being someone who supports somebody else. But no: allies are people who stand by each other and work together.
That’s why we need a trans feminist movement. A trans feminist movements gives people autonomy over their own bodies, space to make their own decisions, and enables people to stand together when we are all at risk.
So I’ll leave you with a chant I want to hear more of at protests:
“Trans rights, women’s rights: one struggle, one fight”.
FOOTNOTES
- My statement here is intended to highlight that more people are out as trans than ever before. Contrary to narratives of “social contagion”, there have always been people with gender diverse or sex nonconforming experiences. What has changed is that there is greater access to information and community, which makes it easier for people to come out. ↩︎
- “During the lifetime of the Review, the term trans has moved from being a quite narrow definition to being applied as an umbrella term to a broader spectrum of gender diversity. This clearly has implications for conceptualisations of detransition” (Cass et al., 2024, p.187). This claim is demonstrably false, as “trans” (and before that, “transgender”) has been used as an umbrella term for decades. This is shown in my own previous work as well as writing dating back to at least the 1980s by individuals such as Leslie Feinberg. ↩︎
- https://wrap.warwick.ac.uk/88285/ ↩︎
- For an excellent, more recent and more detailed analysis on this topic in the context of trans youth healthcare, see Magdalena Mikulak’s (2021) article “For whom is ignorance bliss? Ignorance, its functions and transformative potential in trans health“. ↩︎
- https://growinguptransgender.com/evidence/ ↩︎
- https://www.gold.ac.uk/educational-studies/staff/kennedy-natasha/ ↩︎
- https://www.gla.ac.uk/schools/socialpolitical/staff/harveyhumphrey/ ↩︎
- “Our stance, as gender-affirming practitioners, is that children should be helped to live as they are most comfortable. For a gender-nonconforming child, determining what is most comfortable is often a fluid process, and can modify over time. Therefore, in a gender affirmative model, gender identity and expression are enabled to unfold over time, as a child matures, acknowledging and allowing for fluidity and change” (Hidalgo et al., 2013). ↩︎
- “Since 2018, around 1.77% of young people who are referred to the gender care services at Sandyford have gone on to be prescribed puberty blockers”: https://www.thenational.scot/news/24262271.many-young-people-scotland-given-puberty-blockers/. ↩︎
- Although in practice, trans people are often also turned away from mental health services due to “trans broken arm syndrome“. ↩︎
- In my original speech, I inaccurately stated that the report was “500 pages long”. However, my point about requiring time to carefully consider its contents remains. ↩︎
- “The original published Terms of Reference (ToR) for the Cass Review’s assurance group explicitly excluded trans expertise, stating that it “deliberately does not contain subject matter experts or people with lived experience of gender services” [Report 1, version 1]. The current (updated) assurance group ToR is worded less clearly, yet still conveys exclusion of those with expertise or lived experience, as such individuals would naturally be expected to have an interest in the outcome of the review” (Horton, 2024: p.7) ↩︎
- One former gender clinician was involved in the research process: Tilly Langton, formely of England’s Gender Identity Development Service (GIDS). Langton’s recent activities include promoting conversion therapy materials in training for NHS psychiatrists and lobbying Kemi Badenoch about the UK government’s conversion therapy ban, alongside proponents of conversion practices. ↩︎
- Hilary Cass has contested this claim in reporting for the BBC. Her argument is that of the 103 studies analysed for the review, 60% were included in the synthesis of evidence. However, my argument here is specifically that the findings of these papers were broadly ignored in the writing of the report’s recommendations, while less robust material was instead prioritised. As Simon Whitten argues, “The majority of moderate certainty studies were included in the results section but then arbitrarily ignored in the conclusion entirely”. ↩︎
- I have removed a statement I made about randomised control trials from the transcript here as my point was unclear and therefore potentially misleading (as can happen when you do an unplanned speech on a complex topic!) Unlike the Cass Review team, I am keen to correct my errors. See the links in the above footnotes above for more detailed information on inclusion/exclusion criteria for the Cass Review. ↩︎
- See e.g. https://www.nps.org.au/news/is-paracetamol-effective-for-low-back-pain. ↩︎
- The landscape of evidence anti-psychotics is a complex one. There is “high-quality” evidence that anti-psychotic drugs work better than placebos in addressing various conditions, but the evidence for use of multiple drugs, reducing or increasing doses at particular junctures in treatment, or taking one drug rather than another in treating specific conditions is often of a similar (or lower) quality than the evidence for benefits of endocrine interventions assessed by the Cass Review (see e.g. https://www.sciencedirect.com/science/article/pii/S0890856716319992). ↩︎
- Specifically in the long-term, see e.g.: https://www.nationalelfservice.net/mental-health/adhd/adhd-medications-effective-safe/. ↩︎
- https://onlinelibrary.wiley.com/doi/10.1111/cen.14410 ↩︎
- At this point, somebody stuck their hand up in the audience. I responded: “Someone stuck their hand up and might give me a footnote on that! I totally approve of that. I might invite you up later because I like evidence and I’m obsessed with it. [person indicates they were just waving to their friend, crowd laughs] Oh that’s grand! There we go, we haven’t even had a footnote.” Well, here is the footnote. ↩︎
- p.24 of the Cass Review final report. The rationale for this within the report is that the figure is adapted from a 2018 paper published in Archives of Sexual Behaviour. However, as Trans Actual observe: “The number of referrals to GIDS is known until 2020/21 […] the last 3 years for which data is available, shows that the number of referrals has recently plateaued. Such data is inconvenient for a narrative that relies on an inexplicable explosion in need[.]” ↩︎
- https://transsafety.network/posts/gender-exploratory-nhs-training/ ↩︎
- A historical example of treatment that “tries to make the child comfortable with the sex he or she was born with” within a gender clinic context can be found here: https://www.npr.org/2008/05/07/90247842/two-families-grapple-with-sons-gender-preferences. ↩︎
- p.70, used to evidence the activities of GIDS’ research team at a WPATH conference. They could have instead cited the conference website. ↩︎
- A good summary of the channel can be found in this piece by What The Trans: “When citing a recording from the WPATH 2016 conference, Cass uses a YouTube channel called Thoughts on Things and Stuff. This appears to be the associated channel of a now-defunct blog largely focussed on criticising the Mormon Church. Why this was relevant to Cass is unclear, although titles of recent uploads at the time of the WPATH video include “Dr. Stephen Levine: 13 Untruths Behind Gender Affirmative Therapies for Kids” (Levine is an advisor to Genspect) and “Gays Against Groomers: stop the indoctrination and medicalization of children. 2023 Florida testimony.”, which perhaps provides a clue to how Hilary Cass ended up citing a channel with only 22.4K subscribers. It thus seems that, in addition to being advised by and networked with a variety of prominent anti-trans figures and organisations, Hilary Cass appears to be getting her professional news from homophobic and transphobic YouTube channels.” ↩︎
- Anti-gay campaigners have long attempted to position LGBTIQ+ people as a danger to children. In recent years this tactic has seen a resurgence, through positioning trans and queer campaigners as “groomers”. GLAAD have described Gays Against Groomers as a group who intentionally use “ambiguous messaging about characterizing LGBTQ+ people as pedophiles falsely and maliciously with the absolutely clear intent of driving fear.” ↩︎
- pp.100-101 ↩︎
- https://transsafety.network/posts/bell-v-tavistock/ ↩︎